Urology Pearls: The future of medicine in Vegas — toilet seats and lasers

By DR. SHAHAR MADJAR
Several weeks ago, I wrote here about my visit to the American Urological Association meeting in Las Vegas. I told you about The Strip and the interesting people I had seen along it. I promised to write again about an entirely different world–the one inside the urology meeting, where waves of doctors gather to share their knowledge and visions for the future.
Today, I’ll tell you about two lectures: one focused on a topic of interest mainly to urologists and their patients, and the other–a broader presentation with implications for the future of medicine as a whole.
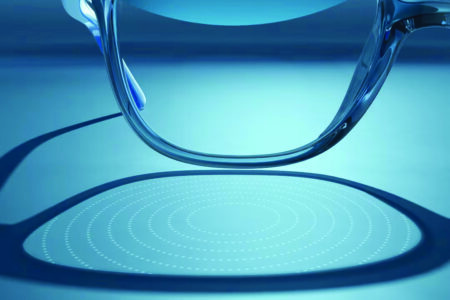
Here is an example of what’s new in urology: about 10% of people develop kidney stones. Smaller stones may pass on their own, but larger stones typically require surgical intervention. Modern urology offers remarkable achievements. With the patient under anesthesia, a urologist can advance a small-caliber camera into the kidney. The camera, only a few millimeters in diameter, is called a ureteroscope. It’s often inserted through a very narrow sheath. Once the ureteroscope is positioned near the stone, the urologist can blast the stone–under direct vision–using a tiny laser fiber, breaking it into small fragments, sometimes as fine as dust. What happens then? The stone fragments may pass on their own, but sometimes they remain in place, coalesce, and form a new, larger stone. And so, the cycle of pain and misery begins again.
At the AUA 2025, a practical solution to this problem was presented: Instead of leaving the fragments and dust behind, the ureteroscope–or the sheath through which it’s passed into the kidney–can now be connected to a vacuum device that suctions these particles out. While the idea of suctioning small stone fragments isn’t new, the technology hadn’t yet been fully developed–until now. A promising solution has emerged.
In another session, Dr. Vin Gupta–a former Chief Medical Officer of Amazon Pharmacy, recognized tech innovation leader, and health policy expert–addressed a broader issue: Despite major advancements in medicine, the prevalence of many chronic conditions has remained unchanged for decades. How can our health system, faced with an aging population and a severe shortage of doctors and medical staff, cope with this challenge? He poses the question to himself and his vast audience–a sea of urologists: “How will we care for more people with fewer people?”
The answer, Dr. Gupta suggests, lies in technological innovation. In an immense lecture hall in Vegas, he paces confidently across the stage. He wears a white shirt, a blue jacket, and no tie. He appears assured and composed. Behind him, slides projected on the screen are larger than life.
He points to the early diagnosis of hypertension as an example. For decades, hypertension has been a major risk factor for disease and disability. Part of the reason, Dr. Gupta claims, is that patients dislike the tools doctors use to screen for it. Nobody enjoys a trip to the doctor’s office. Everyone dreads the pressure cuff! Just thinking about it can provoke anxiety–and … elevate blood pressure.
Dr. Gupta points out that more user-friendly alternatives to the pressure cuff already exist. For example, a hotel-room mirror in Tel Aviv uses photoplethysmography (a light source and a photodetector that measure changes in blood volume with each heartbeat) to estimate blood pressure trends–with surprising precision.
Or consider a toilet seat, aptly named The Heart Seat, that uses a variety of sensors to measure your blood pressure, heart rate, respiratory rate, and oxygen saturation. You sit down on “the throne,” do your business–and the whole time, your vital signs are being monitored, analyzed, and even transmitted to your doctor’s electronic medical record. What a world.
What if, then, your next doctor’s appointment could be scheduled as easily as ordering a book on Amazon–and conducted from the comfort of your home via telemedicine?
These technologies aren’t entirely new. Photoplethysmography is already available on smartwatches and smartphones. While it may not match the accuracy of the traditional blood pressure cuff, it’s widely accessible at a reasonable cost.
As I listened to Dr. Gupta’s lecture, I wondered: Will these and other technologies be enough to motivate people to take better care of themselves? How much of the problem lies in external barriers to care–and how much is buried deep within our own psychology?
Dr. Gupta remains optimistic about the future of medicine.
“I’m giving you the optimistic view of chronic disease management,” he says.
I remain a bit more realistic. I think about the growing need for medical care in a society divided on core values, one that continues to debate how healthcare resources should be allocated. The future is here. But implementing it will take time–and a lot of goodwill.